Contactless Measurement of Heart Rate and Respiration Rate: Transforming Healthcare with Radar Sensors
The demand for compact yet energy-efficient radar sensors for remote vital sign monitoring is witnessing an exponential rise in the healthcare industry for several reasons.
Up to 75% of adverse events and preventable deaths occur due to a lack of multi-parameter vital sign (VS) monitoring in general non-ICU patients [1]. A critical aspect of patient and elderly healthcare is monitoring vital signs such as respiratory rate and heart rate. Most equipment used for tracking, such as ECG and pulse oximeters, require direct skin contact by means of straps and electrodes. They further require cables or periodic charging, thus restricting freedom of movement. However, the advent of cutting-edge radar sensors has spurned new vital sign monitoring techniques that don’t require any physical contact. In this regard, contactless measurement of vital signs is becoming increasingly important as it offers several advantages, including non-contact measurement, continuous monitoring, early detection of irregularities, and seamless integration into consumer-end products.
This article describes the role of radar sensors in improving patient, elderly and health-care outcomes, using Infineon XENSIV™ 60 GHz radar as an example of cutting-edge radar sensor technology.
Understanding Radar Sensors
Radar sensors work by emitting radio waves in the form of electromagnetic radiation. These radio waves travel through space at the speed of light. The emitted radar waves are reflected by objects and people in the environment. With remarkable precision, radar sensors perceive and detect even the minutest movements, enabling a comprehensive monitoring experience.
To detect and measure the subtle movements of the human body, Frequency-Modulated Continuous-Wave (FMCW) radars can be used. FMCW radars use the principles of frequency modulation and the analysis of frequency shifts to enable accurate distance and velocity measurements. The exact mechanism for vital sign monitoring is explained in the following section.
Vital Signs Measurable with FMCW Radar Sensors
Radar sensors can measure the movements of the chest wall during respiration. They detect the subtle changes in the reflected radio waves caused by chest wall displacement during breathing. This technique is known as radar-based respiratory motion detection or radar respiration sensing. Let's understand the basic working mechanism here.
FMCW radars emit continuous waves of radio frequency signals that are modulated in frequency over time. The radar signal consists of a continuous transmission with a gradually increasing or decreasing frequency. This modulation creates a frequency sweep or chirp.
The radar signal is transmitted toward the target (chest), and a portion of the signal reflects back to the radar receiver. This reflected signal, called the echo, contains valuable information about the target object's distance and velocity.
The FMCW method involves emitting a linearly frequency-modulated wave that is subsequently compared with the reflected wave. This process generates a beat or intermediate frequency (IF). The magnitude of this intermediate frequency directly correlates with the distance of the detected object. By accurately measuring this frequency difference or intermediate frequency, the precision of distance measurements is significantly improved. Essentially, the more precise the measurement of this frequency difference, the more precise the resulting distance measurement becomes.
Benefits of Contactless Vital Signs Monitoring
Improved Patient Safety
Traditional wired monitoring systems report heart and breathing rates through combined electrocardiograms and oxygen saturation sensors. Using straps and electrodes in traditional monitoring systems may lead to skin irritation, especially in sensitive patients. The procedure may also cause discomfort for patients with epilepsy or psychiatric problems.
However, radar sensors can enable contactless measurement of vital signs by tracking the position and speed of the chest with built-in antennas. These antennas track breathing and heart-rate movement to report accurate vital signs. This non-contact measurement method neither confines nor inhibits the patient. As a result, there is no discomfort or skin irritation involved.
Patient Convenience
A traditional obstructive sleep apnea diagnosis through full-night polysomnography poses limitations of high cost and first-night effects [9]. If the subject rolls over the bed, it can even cause a potential false alarm.
These sensors work on their own modified echo and are not dependent on any external signal. Additionally, they have the capability to sense through non-conductive materials. This means that it can be hidden behind the product cover, allowing for anonymous operations.
Accuracy and Reliability
Traditional ECGs involve attaching electrodes to the body for heartbeat measurement. However, these electrodes can cause discomfort and alter the natural breathing pattern of the individual, which can introduce inaccuracies in the recorded vital signs. In contrast, patients remain unaware of the measurement during contactless vital sign monitoring techniques. As a result, they are less likely to alter respiration, which directly improves accuracy.
Similarly, during traditional ECGs, contact between the electrode and the skin can introduce surface-loading effects. This leads to changes in electrical properties and potential inaccuracies in the recorded signals. But radar sensors do not exert any pressure on the physical body as they operate with contactless measurement. Thus, the signals obtained remain closer to the natural physiological state, leading to more accurate vital sign measurements.
Scalability
Radar sensors can leverage other technologies, such as AI and sensor fusion, to measure vital signs even in the most challenging healthcare settings, including hospitals, clinics, retirement homes, and even home healthcare environments. They also seamlessly integrate into standard consumer electronics like night lamps, smartphones, tablets, and smart alarm clocks, providing an added health-tracking feature for smart home devices while also serving as a security feature for patients and the elderly.
Compact and Anonymous
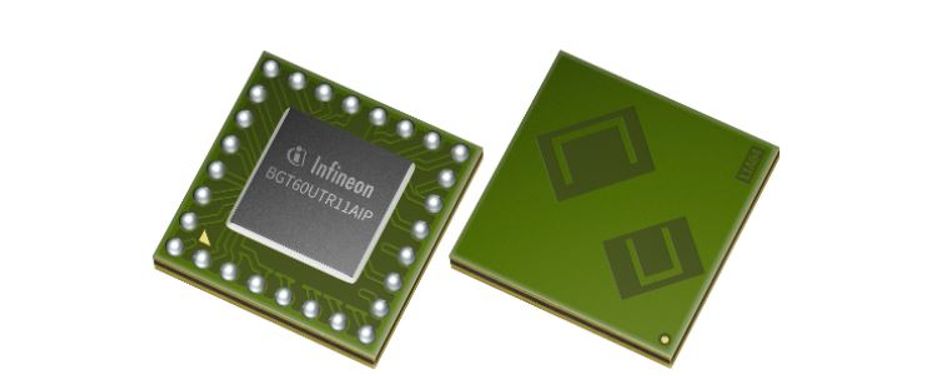
Radar sensors are robust, discrete, and small. They possess the ability to withstand diverse environmental conditions such as temperature variations, lighting changes, humidity levels, dust presence, and more. Moreover, their discreet nature allows them to be concealed behind non-conductive product covers, rendering them virtually invisible to end users. It is important to note that radar sensors do not capture any personally identifiable data, as their signals remain anonymous. Unlike image sensors or microphones, radar sensors do not engage in image or voice recording. As an example, the Infineon XENSIV™ 60GHz radar BGT60UTR11AIP occupies a mere 16 mm² of space. Considering all the necessary components, it can be easily accommodated on a board as small as 2 cm² or even smaller, making it ideal for compact devices.
Applications of Contactless Vital Signs Monitoring
Hospital and clinical settings
Contactless vital signs monitoring can enhance patient care in hospitals and clinical settings. The list includes ICUs, operating rooms, general wards, emergency departments, and sleep centers. For example, radar sensors can continuously monitor patients' vital signs in the ICU without direct contact. Even anesthesiologists and surgical teams can closely monitor patients' physiological responses during OT procedures in real-time. Similarly, integrating contactless vital sign monitoring in general wards eliminates the need for frequent manual measurements. This allows patients to sleep naturally for more accurate and reliable data collection during sleep studies. [2]
Assisted living facilities or nursing homes
Assisted living facilities and nursing homes can leverage real-time monitoring to enable prompt interventions when necessary. Any significant changes or deviations from a resident's baseline vital signs can trigger automated alerts to healthcare providers. Radar sensors can even detect changes in a resident's movement patterns, gait, and posture, allowing for timely interventions. Doctors can contact the patient, diagnose and prescribe medications, and dispatch medical assistance without requiring in-person visits.
Advancements in Radar Sensor Technology
Radar sensors are increasing in functionality by leveraging the power of machine learning, data fusion, and adapting filtering techniques. Machine learning algorithms excel at learning patterns and filtering out noise from complex datasets. They can effectively separate the desired vital sign signals from unwanted noise, leading to improved accuracy. For example, research conducted at SCALE, Singapore has shown that implementing machine learning into mmWave FMCW radar-based non-contact vital signs monitoring systems has improved the accuracy of the relevant vital sign information by filtering out the external noise with ease. [8]
Merging information from multiple radar sensors (data fusion) adds advanced monitoring features [3]. Radar sensors can be combined with optical or accelerometers to achieve more comprehensive and accurate data monitoring. This provides healthcare personnel a more holistic view of an individual's vital signs for better patient management.
To avoid clutter and improve signal quality, adaptive filtering techniques can be used. Two promising techniques are the Least Mean Squares (LMS) algorithm and the Recursive Least Squares (RLS) algorithm. They can be used to suppress noise and interference in radar data.[5] You can also introduce adaptive filtering techniques such as Constant False Alarm Rate (CFAR) detection and adaptive beamforming to further reduce background noise under the threshold level. [6]
When a radar sensor has multiple channels, it can read vital signs from multiple persons in parallel. This expands the scope of its application goes beyond hospitals and nursing homes. For instance, it can be used in the automobile sector to ensure the safety of the driver and co-driver. A multi-channel mmWave radar sensor can continuously monitor for early signs of heart attacks or other cardiopulmonary irregularities in the driver/co-driver.
However, it is worth noting that the application of these techniques depends on the specific characteristics of the radar system, the nature of the signals, and the requirements of the vital sign extraction task.
Challenges and Considerations
The accuracy and reliability of radar sensor measurements can be hampered by various factors. We will examine two significant challenges and discuss strategies to overcome them.
The Amplitude of Body Movements
Rapid body movements during physical activities or tremors can introduce distortions in radar signals, challenging accurate data extraction. For example, when walking around, it is difficult to separate the minor chest movements caused by breathing and heartbeat from the larger movements of the legs and arms. To tackle this challenge, advanced motion compensation techniques can be employed using algorithms such as adaptive filtering, Kalman filtering, or particle filtering [6]. These techniques involve estimating and compensating for the motion-induced effects, enabling more accurate extraction of vital sign parameters.
Absence of Regular Calibration/Validation
Over time, radar sensors may produce erroneous vital sign readings due to factors such as ageing, environmental conditions, or component degradation. To maintain accuracy, it is imperative to conduct regular calibration and make necessary adjustments to the readings to ensure they remain within acceptable limits.
Additionally, it is important to consider the following strategies to enhance accuracy and reliability:
Proper radar sensor placement at a stable and appropriate location to minimize external interferences and maximize signal quality.
Using radome (radar dome) technology to protect the mmWave radar sensors and antenna from external environmental effects such as rain, sunlight, and wind.
Comparing results with established measurement techniques for assessing the reliability and identifying areas for improvement.
Utilizing machine learning and deep learning algorithms to learn patterns and correlations from large datasets for robust measurement.
Improving Radar Sensing with Infineon XENSIV™ 60 GHz radar sensors
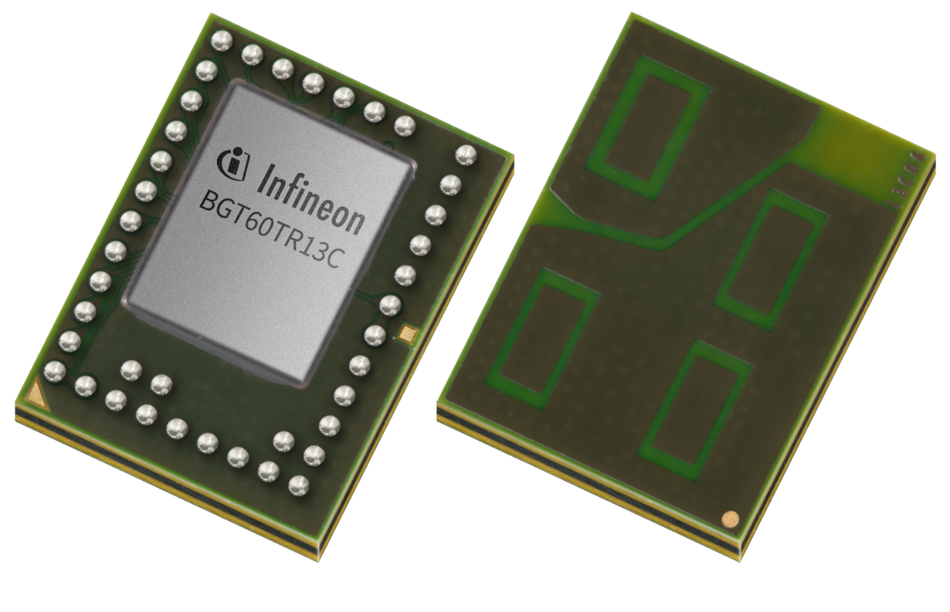
Infineon’s mmWave radar portfolio offers FMCW and Doppler radar sensors for various IoT and automotive applications. The BGT60TR13C and BGT60UTR11AIP 60 GHz radar sensors are particularly suitable for vital sensing (heart rate and respiration rate) at a low cost.
Now let’s look at their key design features for remote vital sign monitoring systems.
Discrete devices
The discreteness of the final package form in vital sign sensing allows for non-intrusive monitoring.
The BGT60TR13C radar sensor features an L-shaped AIP (Antennas-in-Package), whereas the BGT60UTR11AIP radar sensor employs a U-slotted AIP design. Both designs are optimized for compact form factors, ensuring efficient antenna integration. The small package of these sensors helps save PCB area during design and simplifies the overall design process.
Note: The AIP (Antenna in Package) technology refers to an antenna packaging solution that incorporates one or more antennas within an IC package.
| Sensor | BGT60UTR11AIP | BGT60TR13C |
| Integrated Antenna | 1Tx and 1Rx | 1Tx and 3Rx |
| FMCW Bandwidth | 5.6 GHz (57.4 – 63.0 GHz) | 5.5 GHz (58.0 – 63.5 GHz) |
| Ramp Speed | 400 MHz/µs | 400 MHz/µs |
| Size | 4.05x4.05 mm² | 5 x6.5 mm² |
Integrated Finite-State Machine
One of the critical challenges in contactless vital signs measurement is to ensure a network-self-healing mechanism during abnormal body movements of the patients. The BGT60TR13C and BGT60UTR11AIP overcome this challenge with an autonomous connectivity restoration algorithm based on the finite state machine (FSM). With integrated FSM, these radar sensors can autonomously perform chirps, data acquisition, and storage into internal memory. In the event of any abnormal node, it can be replaced with the nearest non-critical node to restore network connectivity seamlessly [7]. This optimized power-switching mechanism ensures minimum power consumption (a few mW on average) during the duty cycle. Further power consumption is achieved through DC duty cycling.
Sub-millimeter Reading
With an incredibly ultra-wide bandwidth (up to 5.6 GHz) followed by a high range resolution (~3 cm), these sensors can detect subtle motions up to a range of 15 m with mm accuracy. This capability is crucial for the early detection of heart attacks or for monitoring the physiological state of patients with critical conditions or those undergoing intensive care. Healthcare professionals utilize this detailed information to customize treatment plans and personalize medications, thereby mitigating critical situations with ease.
Non-obstructive Monitoring
A high SNR (Signal-to-Noise) ratio enables radar sensors to detect movement from a long distance, even in complex healthcare settings where signals and noise from other digital equipment may hamper the readings. Both BGT60TR13C and BGT60UTR11AIP are specifically designed with a high SNR ratio, allowing them to detect subtle chest movements. They can sense vital signs through clothing, bedding, or other non-metallic barriers. This feature makes them suitable for monitoring patients in various settings, such as hospitals or retirement homes, without the need for extensive setup or undressing.
Conclusion
Radar technology provides continuous and non-intrusive vital sign monitoring without the need for body contact. Its utilization in vital sign monitoring is particularly beneficial for elderly and private individuals who are interested in monitoring their vital data in an unobtrusive, robust, discrete, and energy-efficient manner.
Infineon’s 60 GHz radar sensors overcome common challenges such as rapid body movements and external signal interference, ensuring accurate vital sensing.
Feel free to explore further details about Infineon's cutting-edge radar sensor, the XENSIV™ 60 GHz BGT60UTR11AIP, by visiting the following link.
References
1. Weller RS, Foard KL, Harwood TN. Evaluation of a wireless, portable, wearable multi-parameter vital signs monitor in hospitalized neurological and neurosurgical patients. J Clin Monit Comput [Internet]. 2018 [cited 2023 May 30];32(5):945–51. Available from: https://pubmed.ncbi.nlm.nih.gov/29214598/
2. Balasubramanian V, Vivekanandhan S, Mahadevan V. Pandemic tele-smart: a contactless tele-health system for efficient monitoring of remotely located COVID-19 quarantine wards in India using near-field communication and natural language processing system. Med Biol Eng Comput [Internet]. 2022;60(1):61–79. Available from: http://dx.doi.org/10.1007/s11517-021-02456-1
3. Moshawrab M, Adda M, Bouzouane A, Ibrahim H, Raad A. Smart wearables for the detection of occupational physical fatigue: A literature review. Sensors (Basel) [Internet]. 2022 [cited 2023 May 27];22(19):7472. Available from: http://dx.doi.org/10.3390/s22197472
4. Barreto-Cubero AJ, Gómez-Espinosa A, Escobedo Cabello JA, Cuan-Urquizo E, Cruz-Ramírez SR. Sensor data fusion for a mobile robot using neural networks. Sensors (Basel) [Internet]. 2021 [cited 2023 May 27];22(1):305. Available from: https://www.mdpi.com/1424-8220/22/1/305
5. Lampl T. Implementation of adaptive filtering algorithms for noise cancellation [Internet]. Diva-portal.org. [cited 2023 May 27]. Available from: https://www.diva-portal.org/smash/get/diva2:1456739/FULLTEXT01.pdf
6. Wolff D-I (fh) C. False alarm - radartutorial [Internet]. Dipl.-Ing. (FH) Christian Wolff. [cited 2023 May 27]. Available from: https://www.radartutorial.eu/01.basics/False%20Alarm%20Rate.en.html
7. Zhang Y, Wang J, Hao G. An autonomous connectivity restoration algorithm based on finite state machine for Wireless Sensor-Actor Networks. Sensors (Basel) [Internet]. 2018 [cited 2023 May 30];18(1):153. Available from: https://www.mdpi.com/1424-8220/18/1/153
8. Iyer S, Zhao L, Mohan MP, Jimeno J, Siyal MY, Alphones A, et al. mmWave radar-based vital signs monitoring and arrhythmia detection using machine learning. Sensors (Basel) [Internet]. 2022 [cited 2023 Jun 15];22(9):3106. Available from: https://www.mdpi.com/1424-8220/22/9/3106
9. Herbst E, Metzler TJ, Lenoci M, McCaslin SE, Inslicht S, Marmar CR, et al. Adaptation effects to sleep studies in participants with and without chronic posttraumatic stress disorder: Adaptation effects to sleep studies and PTSD. Psychophysiology [Internet]. 2010 [cited 2023 Jul 17];47(6):1127–33. Available from: http://dx.doi.org/10.1111/j.1469-8986.2010.01030.x